Overview
This case model explores the impact of cultural beliefs and interpretations on pediatric healthcare, particularly within a child surgical department. It examines how cultural differences shape medical decision-making, influence doctor-patient relationships, and affect communication between healthcare providers and families.
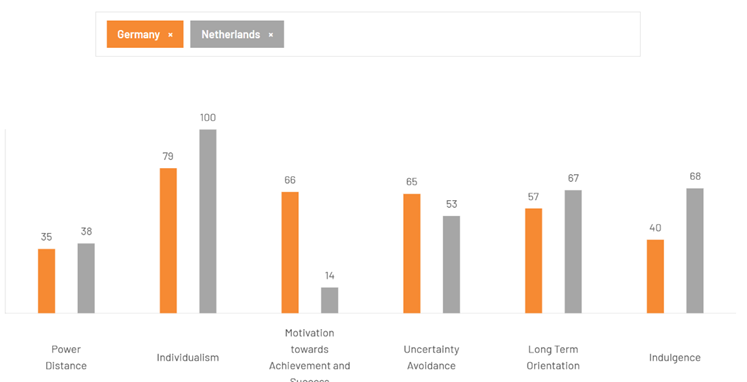
To better understand these dynamics, the study will introduce the Hofstede model as a framework for comparing cultural differences, focusing on key dimensions such as power distance and uncertainty avoidance in medical settings. Insights from our interview with a medical specialist will further illustrate how religious beliefs and cultural perspectives play a role in treatment decisions.
Finally, the study will explore potential solutions to help healthcare professionals bridge cultural gaps. By fostering cultural awareness and improving communication, medical teams can create a more inclusive and empathetic environment, ensuring that every child receives care that respects their family’s values and beliefs.
Hofstede Dimensions
Hofstede’s Cultural Dimensions Theory helps us understand how national culture influences behavior and decision-making. In the context of a German doctor working in a Dutch hospital, these cultural differences can impact healthcare choices, especially when treating sick children. For example, Germany’s higher uncertainty avoidance may lead to a more conservative approach to surgeries, while the Netherlands’ individualism may prioritize parental input and autonomy in medical decisions. Additionally, cultural and religious beliefs can influence treatment options, such as whether to proceed with life-saving surgeries. Understanding these dimensions helps healthcare professionals navigate cultural differences and provide sensitive care.
1. Power Distance Index (PDI)
- Germany has a higher PDI, meaning more hierarchical authority, while the Netherlands values equality and shared decision-making. This could influence the German doctor to adapt to a more collaborative approach with parents and colleagues.
2. Individualism vs. Collectivism (IDV)
- The Netherlands is more collectivist and places more emphasis on the welfare of the collective, while Germany is more individualistic and prioritises personal objectives and liberty. Dutch families may prioritise the family decision, while German doctors may prioritise the requirements of the individual when making decisions about sick children.
3. Uncertainty Avoidance Index (UAI)
- Germany has a high UAI, meaning they prefer clear, structured procedures. In a situation where religion plays a role, like a family’s reluctance to approve a surgery on religious grounds, a German doctor might push for a well-defined, risk-averse approach, emphasizing medical guidelines. In contrast, the Dutch, with lower UAI, might be more flexible, possibly allowing for more discussion with the family about alternative treatments that respect religious beliefs.
4. Masculinity vs. Femininity (MAS)
- Germany leans towards masculinity, focusing on achievement and competitiveness, while the Netherlands is more feminine, emphasizing care, quality of life, and relationships. This could affect how the German doctor approaches patient care, with a focus on efficiency versus a more empathetic, patient-centered approach in the Dutch setting.
5. Long-term vs. Short-term Orientation (LTO)
- Germany has a long-term orientation, focusing on planning and persistence, while the Netherlands has a more short-term orientation, focusing on the present and immediate results. Germany may prioritise long-term health results, whereas the Netherlands may prioritise immediate relief, which could have an impact on how decisions about a child’s therapy or surgery are made.
Outcome
Cultural differences significantly impact pediatric healthcare, shaping medical decisions, communication, and patient care. Hofstede’s dimensions provide a framework for understanding these influences. In Germany, where power distance is higher, doctors often make decisions with minimal family input, whereas in the Netherlands, shared decision-making is prioritized. Some families expect doctors to take charge, while others prefer active involvement in treatment choices.
Cultural values also shape medical approaches. Dutch collectivism emphasizes family-based decisions, while Germany’s individualism prioritizes personal autonomy. German doctors may strictly adhere to medical guidelines, whereas Dutch professionals might explore alternative treatments, particularly when religious beliefs play a role. Some families seek detailed explanations, while others trust the doctor’s expertise without question.
Germany’s efficiency-driven healthcare contrasts with the Netherlands’ patient-centered approach, which values emotional support. Similarly, Germany’s long-term orientation prioritizes future health outcomes, while Dutch practices focus on immediate well-being. Hospitals provide translated materials and interpreters to ensure families from different backgrounds fully understand medical procedures, allowing them to make informed decisions about their child’s care. Accommodating cultural needs helps foster trust and inclusivity.
To achieve the best outcomes for the child, family, and hospital, surgeons must balance medical necessity with cultural sensitivity. This involves clear, empathetic communication and collaboration with cultural mediators when needed. They must align treatments with hospital policies while remaining flexible to patient needs, such as allowing family involvement, adjusting visiting hours, or offering alternative treatment options. By integrating cultural awareness with medical expertise, surgeons can optimize care, ensuring families feel supported while maintaining hospital efficiency and high treatment standards.
Insights from our interview with a medical specialist highlight the importance of cultural awareness in pediatric healthcare. Recognizing diverse perspectives enhances communication, builds trust, and ensures more compassionate and effective care for all families.
Possible solutions
Hospitals can take several important steps to enhance communication and cultural sensitivity in pediatric healthcare. First, they should provide pre-translated medical documents in the primary languages spoken by families, such as consent forms, procedure guides, and post-care instructions. This ensures that all families fully understand their child’s care regardless of their language. Additionally, interpreter services should be readily available, either in-person or via phone/video calls, especially during complex procedures where clear communication is crucial. It’s essential that interpreters are trained in medical terminology to avoid misunderstandings.
Hospitals should also consider the use of cultural mediators or liaisons, who can help navigate cultural differences, particularly around decision-making. Some families may expect a more collaborative, shared decision-making process, while others may place greater trust in the doctor’s authority. Understanding these differences and respecting family preferences can help foster a more positive and inclusive care experience. In cases where families require spiritual support, hospitals can maintain a list of local religious leaders, such as priests or imams, who are available on-call to offer comfort during difficult times.
Flexibility is key to meeting cultural needs. Hospitals should adjust visiting hours, meal options, and communication styles to accommodate family traditions and preferences. A centralized system to manage language services and cultural requests can streamline the process and ensure effective responses. By combining cultural awareness with medical care, hospitals create a more supportive, inclusive environment for families.
Authors
- Karen Abousleiman
International Business, Amsterdam University of Applied Sciences
Block 2, Semester 1, 2025 - Maya Elissawi
International Business, Amsterdam University of Applied Sciences
Block 2, Semester 1, 2025